Parkinson's Disease
Contact Us
Please feel welcome to contact our friendly reception staff with any general or medical enquiry call us.

Parkinson’s disease is the most common form of progressive neurodegenerative disorder with clinical features of slowness of movement, rest tremor, muscular rigidity, and shuffling gait and flexed posture. It is also accompanied by a variety of non-motor symptoms, including sensory, sleep, cognitive, and psychiatric disturbances.

The primary cause of it is widely assumed to be familial.
The Secondary causes of it is due to exposure to drugs, Nutritional toxicity, Hypothyroidism, Infectious
diseases, metabolic causes and Toxic chemicals.
The Secondary causes of it is due to exposure to drugs, Nutritional toxicity, Hypothyroidism, Infectious
diseases, metabolic causes and Toxic chemicals.
The cardinal features of Parkinson’s disease are tremor; a characteristic but not universal component of
the clinical picture. Other symptoms include Rigidity, Akinesia or Bradykinesia( slowing of movements) And postural instability with a tendency to fall. Persons with Parkinson’s disease can show these features in any combination. It’s important also to remember that, at the onset of the disease, the signs and symptoms of Parkinson’s tend to appear asymmetrically.
1. The 'Tremor' of Parkinson’s disease is a characteristic one: it is present at rest, for example, with a
patient’s hands simply placed on his lap. Emotional stress or anxiety tends to worsen the tremor.
intentional movements and sleep inhibit the tremor.
2. 'Bradykinesia' indicates the characteristic slowing of voluntary movements seen in Parkinson’s disease.
(Akinesia can be thought of as a near absence of such voluntary movements). One manifestation of
Bradykinesia is the reduced arm swing during ambulation noted in many patients with Parkinson’s
disease. Another manifestation is the so-called “masked facies” or reduced facial expression seen in
some patients. Many patients have a reduced frequency of blinking that contributes to their unusual
overall facial expression.
3. 'Hypophonia' refers to the soft, sometimes barely audible, speech of many patients with Parkinson’s
disease. Often patients or families notice that the handwriting of individuals with Parkinson’s disease
becomes smaller and less legible over the years; this writing problem is termed ‘micrographia.’
4. In addition to the reduction in arm swing mentioned earlier, Parkinson’s patients develop other gait
peculiarities, including a shuffling quality, and difficulty with starting to walk and stopping while walking.
Some patients with Parkinson’s disease suffer a cognitive decline that can progress to dementia.
the clinical picture. Other symptoms include Rigidity, Akinesia or Bradykinesia( slowing of movements) And postural instability with a tendency to fall. Persons with Parkinson’s disease can show these features in any combination. It’s important also to remember that, at the onset of the disease, the signs and symptoms of Parkinson’s tend to appear asymmetrically.
1. The 'Tremor' of Parkinson’s disease is a characteristic one: it is present at rest, for example, with a
patient’s hands simply placed on his lap. Emotional stress or anxiety tends to worsen the tremor.
intentional movements and sleep inhibit the tremor.
2. 'Bradykinesia' indicates the characteristic slowing of voluntary movements seen in Parkinson’s disease.
(Akinesia can be thought of as a near absence of such voluntary movements). One manifestation of
Bradykinesia is the reduced arm swing during ambulation noted in many patients with Parkinson’s
disease. Another manifestation is the so-called “masked facies” or reduced facial expression seen in
some patients. Many patients have a reduced frequency of blinking that contributes to their unusual
overall facial expression.
3. 'Hypophonia' refers to the soft, sometimes barely audible, speech of many patients with Parkinson’s
disease. Often patients or families notice that the handwriting of individuals with Parkinson’s disease
becomes smaller and less legible over the years; this writing problem is termed ‘micrographia.’
4. In addition to the reduction in arm swing mentioned earlier, Parkinson’s patients develop other gait
peculiarities, including a shuffling quality, and difficulty with starting to walk and stopping while walking.
Some patients with Parkinson’s disease suffer a cognitive decline that can progress to dementia.
These symptoms develop before motor symptoms but are less obvious. The average patient has nine to 12 non-motor symptoms over the course of the disease, such as:
1. Low blood pressure
2. Digestive issues, such as swallowing problems
3. Drooling and/or constipation
4. Urinary issues, such as urgency, frequency and/or retention
5. Mood disorders and/or mental health issues such as anxiety and depression
6. Cognitive changes, such as: Memory loss Difficulty with problem-solving
7. Delusion (believing something that isn’t true)
8. Hallucination (seeing or hearing things that aren’t there)
9. Vision problems
10. Loss of smell
11. Fatigue
12. Sleep disorders
1. Low blood pressure
2. Digestive issues, such as swallowing problems
3. Drooling and/or constipation
4. Urinary issues, such as urgency, frequency and/or retention
5. Mood disorders and/or mental health issues such as anxiety and depression
6. Cognitive changes, such as: Memory loss Difficulty with problem-solving
7. Delusion (believing something that isn’t true)
8. Hallucination (seeing or hearing things that aren’t there)
9. Vision problems
10. Loss of smell
11. Fatigue
12. Sleep disorders
The correct diagnosis of Parkinson's disease is important for prognostic and therapeutic reasons and is
essential for clinical research. In these studies, the most common reasons for misdiagnosis were
presence of essential tremor, vascular Parkinsonism, and atypical Parkinsonism syndromes.
A Neurologist can differentiate Parkinson’s disease from other movement disorders based on different
symptoms and patient history, family history, genetic testing and various other ancillary tests, such
as olfactory testing, MRI, and dopamine-transporter single-photon-emission, computed tomography imaging. All of which help with clinical diagnostic decisions.
essential for clinical research. In these studies, the most common reasons for misdiagnosis were
presence of essential tremor, vascular Parkinsonism, and atypical Parkinsonism syndromes.
A Neurologist can differentiate Parkinson’s disease from other movement disorders based on different
symptoms and patient history, family history, genetic testing and various other ancillary tests, such
as olfactory testing, MRI, and dopamine-transporter single-photon-emission, computed tomography imaging. All of which help with clinical diagnostic decisions.
Stage 1: Individuals experience mild symptoms that generally do not interfere with daily activities.
Stage 2: Symptoms worsen, including tremor, rigidity and other movement symptoms on both sides of the body.
Stage 3: This is considered mid-stage
Stage 4: Symptoms are severe and limiting.
Stage 5: Stiffness in the legs may make it impossible to stand or walk. The person requires a wheelchair or is bedridden. Around-the-clock nursing care is needed for all activities. The person may experience hallucinations and delusions.
Stage 2: Symptoms worsen, including tremor, rigidity and other movement symptoms on both sides of the body.
Stage 3: This is considered mid-stage
Stage 4: Symptoms are severe and limiting.
Stage 5: Stiffness in the legs may make it impossible to stand or walk. The person requires a wheelchair or is bedridden. Around-the-clock nursing care is needed for all activities. The person may experience hallucinations and delusions.
The tell-tale symptoms all have to do with the way you move. You usually notice problems like:
Rigid muscles: It can happen on just about any part of your body. Doctors sometimes mistake early Parkinson's for arthritis.
Slow movements: You may find that even simple acts, like buttoning a shirt, take much longer than usual. Tremors. Your hands, arms, legs, lips, jaw, or tongue are shaky when you're not using them.
Walking and balance problems: You may notice your arms aren't swinging as freely when you walk. Or you can't take long steps, so you have to shuffle instead.
Parkinson's can also cause a range of other issues, from depression to bladder problems to acting out dreams. It may be a while before abnormal movements start.
Rigid muscles: It can happen on just about any part of your body. Doctors sometimes mistake early Parkinson's for arthritis.
Slow movements: You may find that even simple acts, like buttoning a shirt, take much longer than usual. Tremors. Your hands, arms, legs, lips, jaw, or tongue are shaky when you're not using them.
Walking and balance problems: You may notice your arms aren't swinging as freely when you walk. Or you can't take long steps, so you have to shuffle instead.
Parkinson's can also cause a range of other issues, from depression to bladder problems to acting out dreams. It may be a while before abnormal movements start.
Pharmacologically, the drugs used to treat Parkinson’s generally act by working to restore the balance
between the dopaminergic and cholinergic systems. Unfortunately, none of the available drugs has
been convincingly shown to slow the progression of the disease; rather, they improve to greater or
lesser degrees the signs and symptoms only.
All things considered, levodopa is probably the best drug to use in treating elders with Parkinson’s
disease. Levodopa, you may recall, is converted by the body to dopamine, the active agent in nerve
synapses. In order to reduce serious side effects like nausea, hypotension, and cardiac arrhythmias,
levodopa is administered in combination with carbidopa.
Dopamine agonists provide an alternative to levodopa in the treatment of Parkinson’s disease, and are
approved either as monotherapy or as agents that can be used in combination with levodopa. By
combining dopamine agonists with levodopa, you may be able to reduce the dose of the latter drug, and
this often decreases the frequency of dyskinesias or motor fluctuations. Nevertheless, dopamine
agonists as a group have many adverse effects, and many clinicians find that patients with cognitive
impairment tolerate levodopa better.
Amantadine may be useful for persons with mild symptoms, but its tendency to cause confusion or
depression makes it risky to use with older patients. The drug can also cause confusion, not to mention
agitation, restlessness, urinary retention, constipation, and dry mouth.
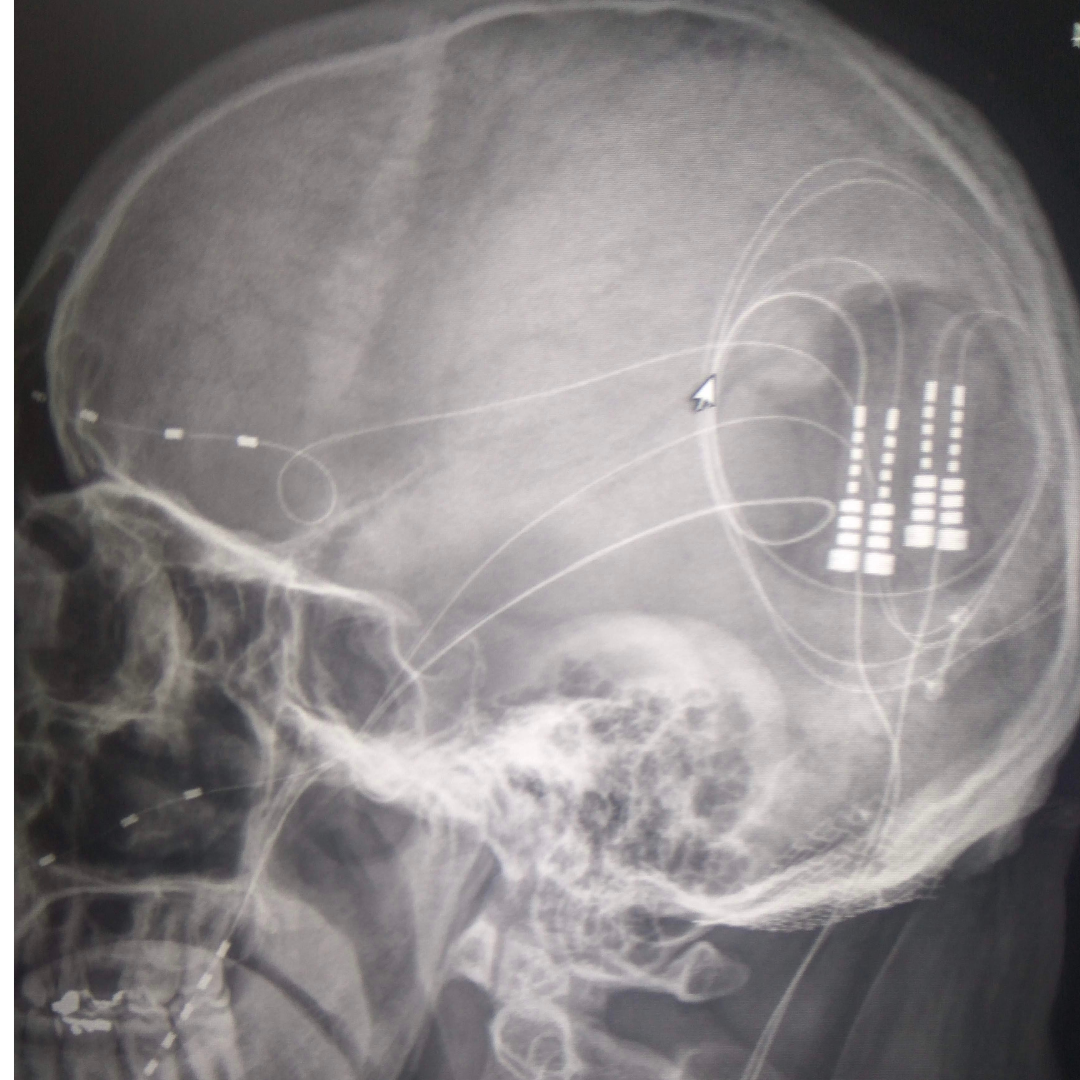
Various surgical treatments exist for Parkinson’s disease, although they are seldom used in the
treatment of frail, elderly patients. Pallidotomy – in which selected tissues are resected or destroyed,
and deep brain stimulation, which involves the careful placement of electrodes in selected areas.
Patients who might be good candidates for these procedures have the following characteristics: They
are cognitively intact; they still show a response to dopaminergic drugs, although their motor symptoms
have been progressing; and they are vigorous enough to withstand the procedures. Patients who
appear to be good candidates and who might consider such treatments should be referred to a
neurologist who specializes in Parkinson’s disease for an evaluation.
Other treatments are crucial for optimal management of Parkinson’s disease. Physical therapists
provide important gait training and strengthening exercises, as well as with selection of appropriate
devices to assist with ambulation. Exercise has been shown to help with mood, strength, flexibility, and
mobility. Occupational therapists are also very helpful in the provision of training and assistive devices
for daily living activities like eating, bathing or showering, toileting, and so forth. Many Parkinson’s
patients with difficulties speaking or swallowing, or with drooling problems, may benefit from speech
therapy consultation.
between the dopaminergic and cholinergic systems. Unfortunately, none of the available drugs has
been convincingly shown to slow the progression of the disease; rather, they improve to greater or
lesser degrees the signs and symptoms only.
All things considered, levodopa is probably the best drug to use in treating elders with Parkinson’s
disease. Levodopa, you may recall, is converted by the body to dopamine, the active agent in nerve
synapses. In order to reduce serious side effects like nausea, hypotension, and cardiac arrhythmias,
levodopa is administered in combination with carbidopa.
Dopamine agonists provide an alternative to levodopa in the treatment of Parkinson’s disease, and are
approved either as monotherapy or as agents that can be used in combination with levodopa. By
combining dopamine agonists with levodopa, you may be able to reduce the dose of the latter drug, and
this often decreases the frequency of dyskinesias or motor fluctuations. Nevertheless, dopamine
agonists as a group have many adverse effects, and many clinicians find that patients with cognitive
impairment tolerate levodopa better.
Amantadine may be useful for persons with mild symptoms, but its tendency to cause confusion or
depression makes it risky to use with older patients. The drug can also cause confusion, not to mention
agitation, restlessness, urinary retention, constipation, and dry mouth.
Various surgical treatments exist for Parkinson’s disease, although they are seldom used in the
treatment of frail, elderly patients. Pallidotomy – in which selected tissues are resected or destroyed,
and deep brain stimulation, which involves the careful placement of electrodes in selected areas.
Patients who might be good candidates for these procedures have the following characteristics: They
are cognitively intact; they still show a response to dopaminergic drugs, although their motor symptoms
have been progressing; and they are vigorous enough to withstand the procedures. Patients who
appear to be good candidates and who might consider such treatments should be referred to a
neurologist who specializes in Parkinson’s disease for an evaluation.
Other treatments are crucial for optimal management of Parkinson’s disease. Physical therapists
provide important gait training and strengthening exercises, as well as with selection of appropriate
devices to assist with ambulation. Exercise has been shown to help with mood, strength, flexibility, and
mobility. Occupational therapists are also very helpful in the provision of training and assistive devices
for daily living activities like eating, bathing or showering, toileting, and so forth. Many Parkinson’s
patients with difficulties speaking or swallowing, or with drooling problems, may benefit from speech
therapy consultation.
Deep Brain Stimulation (DBS) be often described as pacemaker for the brain, sending electrical signals to the brain. During DBS surgery, Neurosurgeons use microelectrode recording and various advanced techniques to place the electrode in correct place. The electrodes are connected to a generator implanted in your chest near your collar bone. The lead delivers electrical currents responsible for movement, regulating the abnormal brain cell activity that causes symptoms such as tremor and gait problems and may reduce your Parkinson's disease symptoms.
Over successive programming DBS improves shaking, Stiffness, Slowness, Painful cramping, Involuntary movement. When DBS is ‘on’ its acts like an electronic dopa which helps in reducing the dose of medication and their side effects. DBS can also improve Mood, Energy level, General sense of well-being. However there is no data which shows that it slows down the disease progression.
In general, if you have had Parkinson's disease symptoms for at least three years, good response to Parkinson's disease medications, especially Carbidopa/Levodopa, “On/Off” fluctuations, have tried other Parkinson's disease medications, such as Entacapone, Tolcapone, Selegiline, Apomorphine or Amantadine without beneficial results and Parkinson's disease symptoms that interfere with daily activities are the best candidates for DBS surgery At KIMS Hospitals patients are being evaluated by the Parkinson’s group which has professional training in DBS. The Parkinson’s group includes a Functional Neurosurgeon, Movement disorders specialist, Clinical Neuropsychologist, Physiotherapist, Nurse and other medical team members evaluate and decide whether you are fit for DBS or not.

The Parkinson’s Group improves life for individuals with Parkinson’s Disease by improving care and advancing research towards a cure. In all that we do, we expand on energy, experience and passion of our worldwide Parkinson’s group.